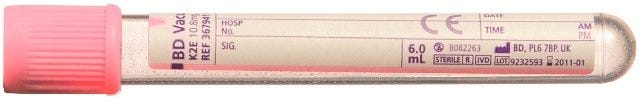
Here’s a familiar scenario. You’ve found a patient who has a low Hb and needs a transfusion so you go through the trouble of taking a single group and save…
Twenty minutes later you take another sample and you send it off…
Oh let’s not forget the most painful part of it all. That is having to handwrite the patients details, in an age where computers do everything!
After sending the sample, you get a ring from the lab to tell you that one sample has been rejected because you’ve missed something on the label. Damn it!!
Now you have to put everything down and take another sample to the disappointment of the patient :(
Over the past few years, we’ve been hit with some scandals. For example, the COVID PPE scandal where it was found that the quality of the equipment wasn’t up to scratch was one such scandal where quality control was poor. However, the blood transfusion scandal has resulted in the deaths of many.
This article is a summary of a number of articles which can be read on BBC News.
What is the Blood Transfusion Scandal?
This refers to a series of transfusion related HIV and Hepatitis C infections that were contracted by patients in the 1970s. Two groups were affected. The first were patients with haemophilia receiving transfusions and the second were patients who were given blood transfusions for generalised reasons such as after childbirth, surgery or simply, low Hb.
Overall, it’s expected that almost 39,000 patients were infected with up to two-thirds of patients with haemophilia who received the transfusion, dying due to Aid’s related illness.
Why Did it Happen?
Similar to the COVID PPE scandal, there was a huge demand of resources acutely. In the 1970s blood products were hard come by so the UK decided to purchase supplies from the US. Much of this blood came from high-risk donors such as prison inmates and drug-users and it’s unsure as to whether those involved knew this at the time.
Blood screening wasn’t a thing then and blood came in batches. So even if one person had HIV, it would mean that the entire batch of blood would be contaminated!
How Did The Government React?
Around 1980, it was realised that imported factor VIII (for haemophiliacs) showed cases of contamination. HIV research was quite preliminary at this stage and the government denied that HIV was being transmitted in these products. The UK proceeded to continue importing blood products and it was only in 1985 that imported factor VIII started to be “cleansed” of viruses.
However, RBC blood products were still contaminated.
What’s Happening Now?
After years of noticing the high rates of HIV and hepatitis C from those who received blood transfusions around 1970, an independent enquiry was set up in 2017. Patients had been campaigning for decades with testimonies from patients, haematologists and others who have been affected by this terrible scandal. The government has agreed to provide compensation to the families and children who have been affected, but a final settlement is yet to be agreed.
So What Can We Learn From This?
So I’ve been reading around this case a lot and have extracted some vital lessons. It links back to patient safety and quality care but ultimately, the cause isn’t always straight forward:
This case is an example of multi-system failure. From the lack of blood products in the UK, to the suppliers in the US and also those who were responsible for overseeing the safety of blood products. Putting the blame on a single entity is difficult although it is clear the government didn’t take the concerns of those affected seriously.
If something isn’t up to scratch, don’t use it! I was recently administering joint injections and found that the blue needle I normally use for shoulders were blunt. I realised that all the needles from that particularly batch were blunt! I didn’t let it slide and instead let the ward manager know who assured me that she would escalate it to supplies and logistics.
Procedures are there to be followed. Taking two group and saves is annoying, especially when you have to write the details on both bottles. However, there is ample research on why this has become the gold standard way in which we can ensure safe transfusion.
Be a blood donor! Donating blood is an awesome way of giving back to the healthcare system. It doesn’t take much and you even get free crisps and a chocolate whilst donating!
Until next time..
E-books, E-books and more E-books
We at Pareto have been busy researching and writing a number of e-books for you all! Our principle is to produce high-yield knowledge and we aim to help you all in your clinical journeys.
Our latest e-book is titled “mastering antibiotics” and will teach you the core principles of antibiotic selection and prescription.
You can find out more and purchase here
Check us out on our various pages
Website: www.paretoeducation.co.uk
Instagram: www.instagram.com/pareto_ed
Twitter: www.twitter.com/pareto_ed
Youtube: https://bit.ly/3DPm23c
Email: paretopaeducation@gmail.com