Flu season is pretty crazy this year. I feel like all I see is patients with flu in A&E at the moment and there are certainly no immediate signs that things are going to change.
For those with a background of asthma/COPD - flu can act as a significant trigger. Not to mention that Covid-19, RSV and bacterial organisms are also floating around. In this update I want to talk about COPD and an interesting finding I came across.
COPD is fairly well understood but is hard to manage. To oxygenate or not to oxygenate, is the patient a CO2 retainer, does this patient have features of asthma? These questions are quite common in patients with COPD.
One common concern is over-oxygenation. The current understanding is that one should establish if someone has a baseline normal CO2 (normocapnia) or high CO2 (hypercapnia) which helps to determine the presence of CO2-driven breathing. In hypercapnic patients, the advised oxygen target is 88-92% to prevent over oxygenation and compromising the CO2 drive.
So we have two separate oxygen scales. 94-98% for normocapnic patients and 88-92% for hypercapnic patients. Confusing. Over oxygenation remains an issue with COPD patients with 25% of patients on non-invasive ventilation being put on NIV due to inappropriate ventilation. This tells you that despite the years of education and experience, this still remains a huge issue.
A recent, observational study that surveyed 2645 patients with COPD in the UK found that oxygenation, regardless of background CO2 levels is detrimental to health outcomes. In other words - SATs over 88% in any individual with COPD is a good thing. Nice and simple?
This is quite a good study. The sample size was large enough with inclusion of patients who had COPD strictly confirmed via spirometry. Like with most observational studies however, causality cannot be proven. There is no longitunal data to pick up on trends therefore only establishing an association but not causality. However, these results are in keeping with high quality randomised control trials (RCTs) that are out there.
So how does this change my practice? I’ll simply be aiming all my COPD patients to be > 88% SATs. This is the approach the British Thoracic Society (BTS) is moving towards anyway as more data is released but it still recommends different oxygen scales. I like simplicity and there are plenty of studies demonstrating the harms of oxygen despite the stated aim for the oxygen saturations.
Hope you found that useful. Oh.. and happy new year!
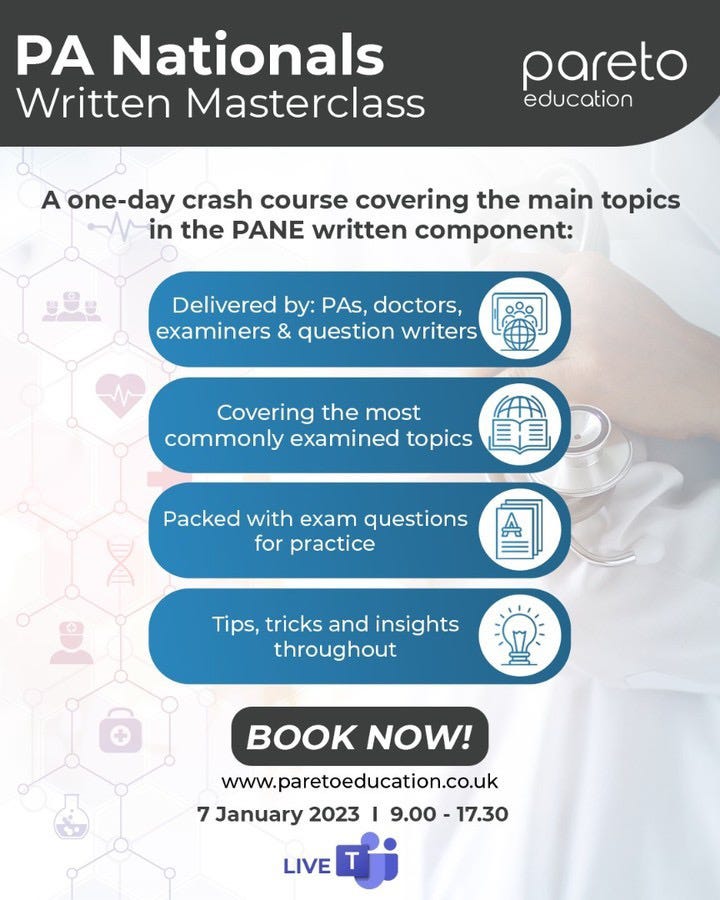
If you’re a physician associate due to sit your national exams soon (Jan or Sept 2023) then be sure to sign up to our written masterclass. The content will also be hugely beneficial for other allied health professionals as we will be covering the core medical/surgical specialties.
Spaces are limited so book now!
Check us out on our various pages
Website: www.paretoeducation.co.uk
Instagram: www.instagram.com/pareto_ed
Twitter: www.twitter.com/pareto_ed
Youtube: https://bit.ly/3DPm23c
Email: paretopaeducation@gmail.com