Holding the on-call gynae bleep always brings through some interesting cases. I’ve done it a few times and have received phone calls from GPs, A&E and other specialties requesting some gynae advice.
The main theme on most days is uterine fibroids. The queries go a little bit like this…
Patient X is 40, has heavy PV bleeding, can she come to you for assessment for ?fibroids
Patient Y has a low Hb and ferritin. She said she has intermittent bleeding. Maybe she has ?fibroids
Patient Z has deep pelvic pain and bloating. She is of a Afro-Carribean origin and her pain is very bad. If you could kindly assess her for ?fibroids
So I thought I’d dedicate this weeks issue to some information about uterine fibroids.
The Psychological Effect of Fibroids
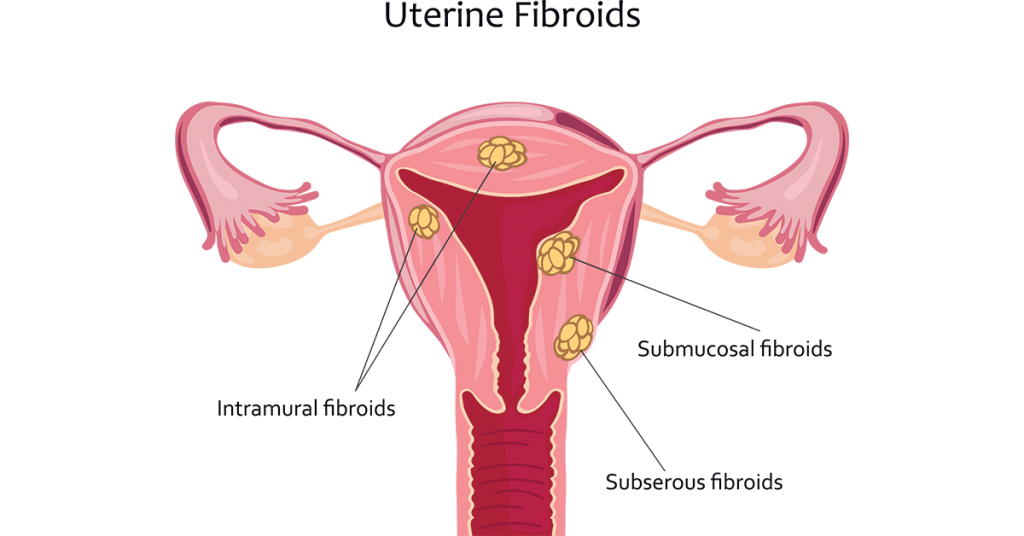
Fibroids are non-cancerous growths that grow in the muscular wall of the womb. They grow due to the normal circulating hormones such as oestrogen and progesterone.
Most women don’t know they have fibroids until later on in life as they start to cause symptoms. This is typically around 40 years old until perimenopause due to the gastric changes in hormone levels. Symptoms typically include:
PV Bleeding
Pressure in the pelvis due to their size
Pain.
Some women present with symptoms of anaemia such as tiredness and can be found to have profoundly low levels of haemoglobin which can point to fibroid bleeding.
Whilst it is a chronic disease, patients with known fibroids can present acutely to A&E or gynaecology assessment units. Multiple studies have looked into why this is and it is due to the mental health impact of fibroids. The symptoms are always present and can cause significant discomfort. Studies have found women with fibroids to have a reduced quality of life and significant distress, both of which are exacerbated in ethnic minority patients.
This means fibroids are from being “minor'“
How Can We Treat Fibroids?
The first is to recognise what fibroids can and can’t do to the body. For instance,
Fibroids CAN NOT cause sudden, large volume PV bleeding
Fibroids CAN NOT cause a sudden acute abdomen.
Fibroids CAN cause profound microcytic anaemia due to a long period of bleeding.
Most patients with known fibroids are simply fed-up with their symptoms. Despite extensive outpatient follow-up, they will still seek treatment. You may find patients may have been offered hormonal treatment which have been refused as patients are looking to conceive. Fibroid treatment is multi-layered and requires a holistic approach.
For first presentations, fibroids can be diagnosed using an ultrasound scan. There are some treatments you can initiate acutely whilst the patient waits for an outpatient gynaecology appointment:
If bleeding is a problem, you can trial Tranexamic acid or an NSAID
If the patient is open to having contraception then the combined contraceptive pill or a Mirena coil are plausible options.
Other options include:
Gonadotrophin-releasing hormone (GnRH) agonists: These can reduce the size of fibroids significant but can revert back to their original size once treatment is stopped
Surgery: This can involve a myomectomy, laparoscopic removal of fibroids or a hysterectomy.
Hope this summary has been useful. If there are any other topics you’d like an insight into then let us know!
Until next time
Check us out on our various pages
Website: www.paretoeducation.co.uk
Instagram: www.instagram.com/pareto_ed
Twitter: www.twitter.com/pareto_ed
Youtube: https://bit.ly/3DPm23c
Email: paretopaeducation@gmail.com