Profuse vomiting, watery diarrhoea, and crampy abdominal pain...
On examination: a tender abdomen, the patient writhing in pain, and noticeably febrile to the touch.
“I had a takeaway pizza last night, Doc.”
Gastroenteritis.
There it is—the diagnosis we all appreciate, not because it's glamorous, but because it offers a clear explanation for a condition that causes significant distress.
However, gastroenteritis isn’t always viral, and the latest listeria outbreak in the USA is a stark reminder of this. So far, three people have died and one pregnancy was lost. The source? Chicken sold at Walmarts across 13 states.
If you think back to high school science lessons about cholera and how the outbreak was traced in 19th-century London, the investigative approach remains strikingly similar. More cases are emerging, and the US Centers for Disease Control and Prevention (CDC) is actively tracking the outbreak.
As clinicians, while gastroenteritis might feel like a “comfort diagnosis,” it’s important to remain vigilant for red flags that warrant escalation. Listeria, for example, can cause serious systemic illness, including seizures. Some pathogens present with bloody diarrhoea, while others have longer incubation periods, delaying symptom onset.
Below is a quick refresher on key bacterial causes of gastroenteritis, along with their clinical features. We hope this summary supports your clinical reasoning. References include the Oxford Handbook of Clinical Medicine and guidance from the Royal College of Emergency Medicine.
E. coli (Enterotoxigenic E. coli – ETEC)
Common form: Traveller’s diarrhoea
Key History: Recent travel to developing countries - suspect if they’ve eaten street food
Onset: Gradual, 1–3 days after exposure
Symptoms: Watery diarrhoea, abdominal cramping, no blood
Treatment? Normally self limiting
Bacillus cereus
Key History: Reheated rice dishes (esp. fried rice from takeaways). Particularly common in East Asia.
Onset: Rapid onset
Symptoms:
Patients will either have diarrhoea or vomiting, rarely both. May also be accompanied by cramps abdominal pain.
Treatment?: Short-lived illness; classic food poisoning story
Salmonella (non-typhoidal)
Key History: Undercooked poultry, eggs, or unpasteurized milk. Prawns is a big one!
Onset: 6–72 hours
Symptoms: Watery or sometimes bloody diarrhoea along with the other symptoms associated with food poisoning.
Source: Contaminated food (poultry, eggs, dairy)/
Treatment?: Often febrile, high temperatures, may require admission as can be unwell.
Shigella
Key History: Daycare exposure and poor sanitation. Quite common in homeless populations.
Onset: 1–3 days
Symptoms: High fever, bloody and often mucus-filled diarrhoea. Quite nasty looking stuff.
Source: Fecal-oral transmission, contaminated water
Treatment? Severe cramping, patients often shocked with appearance of stools. Can cause seizures in children.
Listeria monocytogenes
Key History: Consumption of deli meats, soft cheeses, unpasteurized dairy. Think history of RAW foods.
Onset: Few days to several weeks. Very slow onset.
Symptoms: Mild gastroenteritis OR invasive disease (meningitis, fetal loss). Be careful in those who are immunocompromised
Source: Ready-to-eat meats, unpasteurized dairy
Treatment? Pregnant women, elderly, and immunocompromised at high risk for invasive disease
Campylobacter jejuni
Key History: Similar to Listeria = undercooked poultry, raw milk, or contaminated water
Onset: 2–5 days
Symptoms: Fever, crampy abdominal pain, bloody diarrhoea. Can also present with neurological symptoms such as pins and needles in patients. This would indicate complications like Guillain-Barré syndrome.
Source: Poultry, waterborne outbreaks
Treatment? Can mimic appendicitis. Safety net for neurological symptoms if suspected.
Clostridioides difficile (C. diff)
History Clue: Recent antibiotic use (especially clindamycin, cephalosporins, fluoroquinolones), hospital stay
Onset: Within days to weeks of antibiotic exposure
Symptoms: Profuse watery diarrhoea, pseudomembranous colitis, fever, leukocytosis
Source: Endogenous flora or healthcare environment
Notable: Nosocomial; can be recurrent or severe (toxic megacolon)
Some final thoughts…
History is key with regards to the various presentation of gastroenteritis. With all these cases, regardless of principle be sure to cover the following points:
Gastroenteritis is a clinical diagnosis, only investigate if needed!
DO NOT blindly prescribe antibiotics. Request a stool culture if diarrhoea persists after 7-10 days.
Safety net all patients for blood in stool, high temperatures, intractable vomiting/diarrhoea and rigors. Patients with any of these features will require immediate attention.
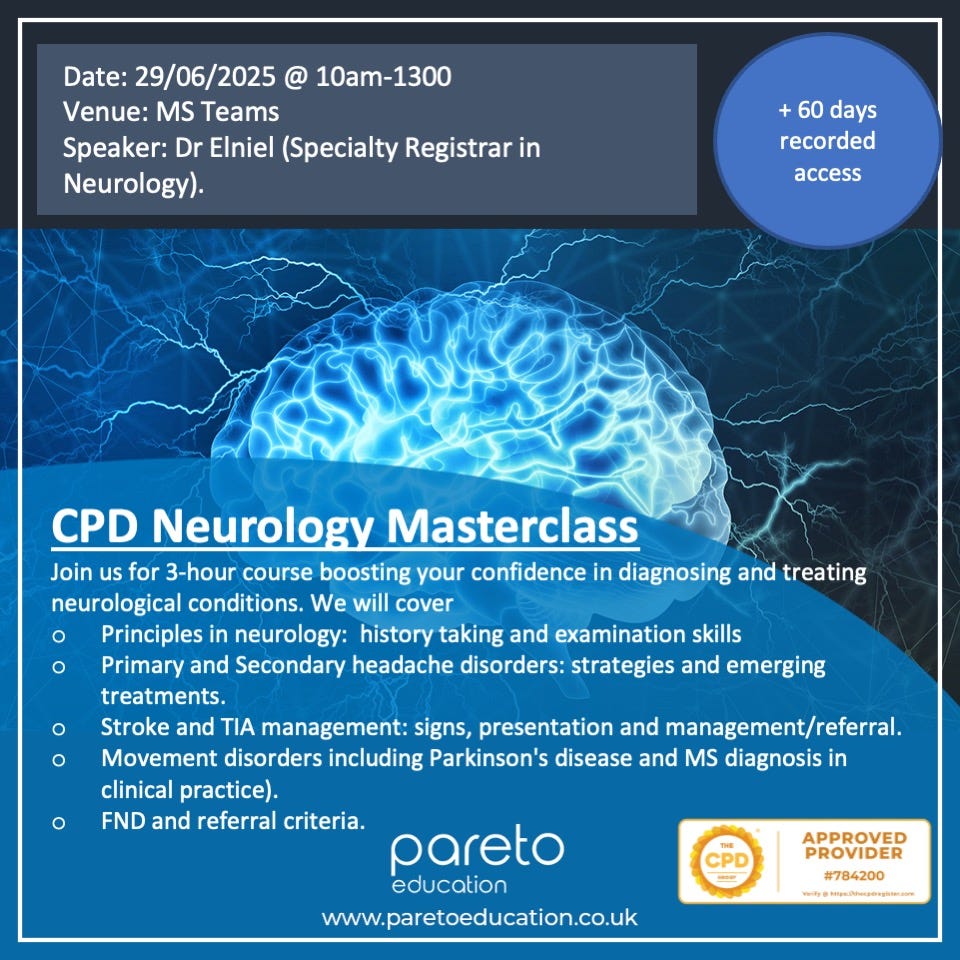
Neurology is Tough..
I’m not wrong, am I? Neurology is traditionally one of the trickiest specialties and it can very difficult to differentiate between presentations and decide that’s an emergency and what isn’t.
It is for this reason that we have invited Dr Elniel, a doctor in neurology who will deliver a carefully designed neurology masterclass. The topics covered include:
- Principles in neurology: history taking and examination skills
- Primary and Secondary headache disorders: strategies and emerging treatments.
- Stroke and TIA management: signs, presentation and management/referral.
- Movement disorders including Parkinson's disease and MS diagnosis in clinical practice).
- FND and referral criteria.
As always, the event is held LIVE and will be RECORDED for future viewing. You will also receive an external accredited CPD certificate. You can book here.
Primary Care is Moving Fast.. Are YOU Moving With It?
If you haven't noticed, the NHS is being restricted. Jobs are scarce, budget cuts are widespread and AI is coming to the NHS. All of this is to try and re-focus healthcare towards primary prevention and it is important that we as clinicians continue to ride the wave.
It is for this reason we created this video titled “Top FIVE Areas to UPSKILL in Primary Care”. We take a look at the latest stats and NHS policy documents and uncover the key areas you need to focus on as part of your CPD.
Website: www.paretoeducation.co.uk
Instagram: www.instagram.com/pareto_ed
Twitter: www.twitter.com/pareto_ed
Youtube: https://bit.ly/3DPm23c
Email: info@paretoeducation.co.uk