I recently assessed a patient who was incredibly depressed. I don’t mean low mood, but pathological depression where her confidence was knocked for six. She was previously a highly functional mother of three but for a few years, her mood has taken a massive tumble.
What’s the cause you might ask? It was a diagnosis of Hidradenitis suppurativa (HS). Now, it’s not the first time I’ve come across the disease of course. I’ve prescribed treatment, referred to dermatology and even drained abscess’ but this lady was particularly bad and her options were running out.
What is HS and why does it happen?
Hidradenitis suppurativa is a chronic skin condition characterized by painful, inflamed lumps, usually in areas where skin rubs together, like the armpits, groin, or under the breasts. These lumps can break open, releasing pus, and may lead to scarring. The exact cause is unclear, but it’s thought to involve hair follicle blockages and an abnormal immune response.
It’s considered an auto-inflammatory condition. This is different from auto-immune as there is purely a rise in inflammatory markers as opposed to an increase in antibody production. For example, studies have found elevated levels of pro-inflammatory cytokines like TNF-α, IL-1, and IL-17 are found in the skin. This inflammatory response isn’t always due to bacterial infection (although this can happen) and therefore, abscess’ can form without underlying infection.
Further risks of HS
Identifying HS is very important not only to manage the disease but also the associated complications. The heightened state of inflammation can increase the risk of the following diseases:
Obesity, metabolic syndrome, Type 2 diabetes and CVD
Inflammatory arthritis - patients have a 65% increased risk of axial spondlyoarthritis (refer to clinical features), a 44% increased risk for psoriatic arthritis and a 16% increased risk for rheumatoid arthritis
Needless to say that the disease can also increase the risk of mental health problems such as anxiety and depression. This is down to the appearance of the disease as well as the repeated need for treatment and even surgical procedures.
Immediate complications can also be serious including sepsis and lymphoedema. It is clear that the disease can become very serious.
What are the treatment options?
Treatment can be split depending on the severity of the disease as well as the manifestation (abscess etc) of the disease. Here are some broad principles. If you want some more detailed information then refer to this document by PCDS.
For mild disease consider a topical clindamycin bd or prescribe oral doxycycline 200mg od; both initially for 3 months. Other options include oral rifampicin 300mg bd.
Other options include spironolactone or metformin. Whilst they are unlicensed, there is some evidence to suggest that they can help with worsening disease.
Managing complications: clinicians are asked to consider testing for FBC, LFTs, HBA1c and serum lipids.
For any acute flares of disease, patients should be given oral antibiotics such as flucloxacillin.
When should referral be considered?
Similar to acne, the referral criteria is more to do with complicated scenarios e.g. pregnancy and impact on psychological health. Referral should also be made for patients with any scarring. For clinicians in primary care, it’s certainly worth starting an advice and guidance (A&G) conversation first to see if referral is required or not.
So what does secondary care do?
Perhaps the main option on the table are biologics. These are the future of pro-inflammatory and auto-immune disease management and currently Secukinumab is licensed for moderate to severe HS in the UK. The current targets of treatment include:
a reduction of 25% or more in the total abscess and inflammatory nodule count, and
no increase in abscesses and draining fistulas.
So what happened to my patient? Turns out she had been seen with a GP with special interest in dermatology and was already started on spironolactone and rifampicin. Unfortunately she continued to have abscess’ and has now been referred for biologics. I sincerely hopes she gets better!
Until next time…
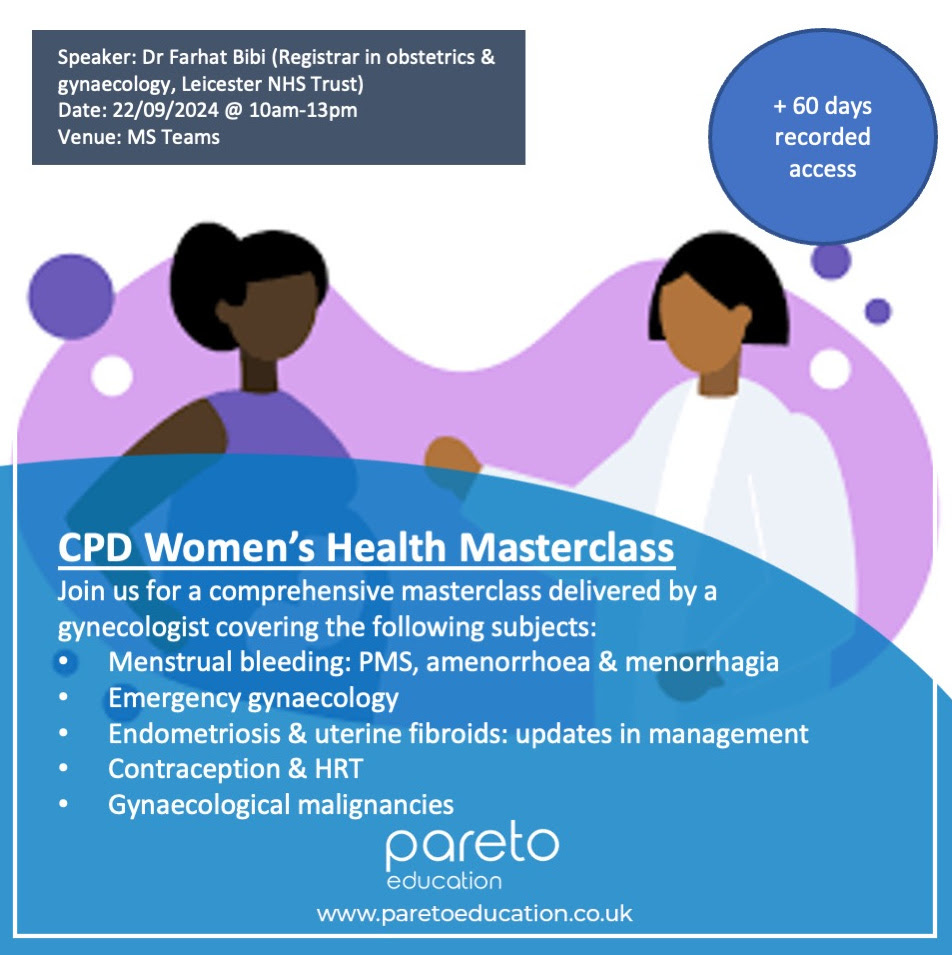
CPD Women’s Health
Join us on 22/09/2024 where we host Dr Farhat Bibi, gynaecology registrar who will cover some key topics related to women’s health. These will include:
Managing PV bleeding in the acute setting
HRT counselling, prescription and follow up,
Endometriosis & uterine fibroids: updates in management
Safeguarding in gynaecology
Gynaecological malignancies
You can book here: https://www.paretoeducation.co.uk/service-page/cpd-women-s-health-masterclass
Check us out on our various pages
Website: www.paretoeducation.co.uk
Instagram: www.instagram.com/pareto_ed
Twitter: www.twitter.com/pareto_ed
Youtube: https://bit.ly/3DPm23c
Email: paretopaeducation@gmail.com