The practice I work at isn’t particularly big but contains within it a wide variety of clinicians who have experience in several fields. This includes drug and alcohol services, homeless medicine and I even have a colleague who is a qualified mathematician.
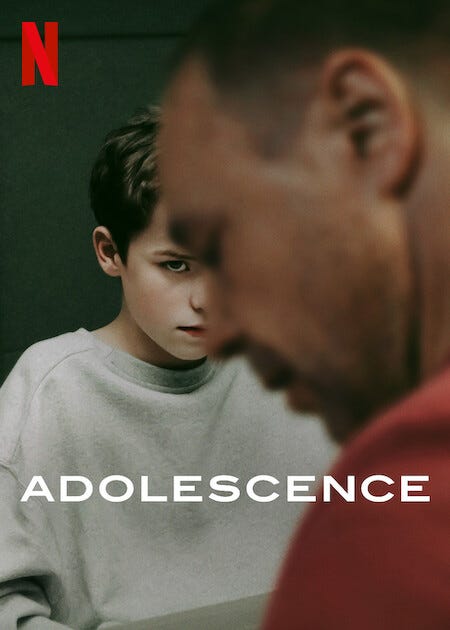
I recently was in conversation with Alice, an ACP who works for the UK prison service. She works at one of the largest HMPs in the country and through her experience has moulded her practice to deal with really dark cases. The conversation started after we spoke about the recently Netflix show Adolescence (*** SPOILER ALERT***) where the main character is taken into prison and is subject to quite an intrusive medical. She shared some really interesting insights into some of the challenges of working in prison. She described prison as a medley of contrasting concerns - a world where medicine meets security, ethics clash with control, and care is shaped by constraint.
Here are some of her insights:
Prescribing Behind Bars
Alice is a prescriber so I asked her what prescribing was like. She mentioned that each prescription is really scrutinised and in most cases, requests have to be made early so they can be discussed at an early morning briefing each day. Many of these patients have complex medical and psychiatric needs and thus, mental health services are either in house or only a phone call away.
For chronic illness’, the challenge is medication adherence and how medication goes “missing.” It’s well known that inmates would use anything as currency to try and obtain cigarettes, additional food items and in some instances, drugs.
“Are inmates particularly violent?” I asked..
“No, but they can be very manipulative…” Alice replied.
The Subtleties of Manipulation
It became clear to me that working as a healthcare professional in prison wasn’t for everyone. You had to be quick on your feet, witty and sensitive to any form of manipulation taking place. Alice mentioned that incarcerated patients would often use their healthcare to obtain certain concessions including more time outside, isolation and sometimes just a quieter place to sleep.
“Some will claim chest pain or seizures, not for medical help, but to be escorted to another wing to settle a score, avoid a threat, or make a drug connection…” She said.
The difficulty is managing the reaction of the patients. As mentioned above, these patients can be severe mental health issues so it can be difficult to differentiate a genuine need and delusional behaviour. These patients will not stand “no” for an answer and thus require a round about way to manage their expectations.
Drug Seeking in a Controlled Environment
Much of the insight we obtain about prison life is from American TV. British prisons are assumed to be simpler and with better controls but according to Alice, the problems are one in the same. As many incarcerated patients are bought in with some use of restraint, one of the most common presentations is limb injury. There are also cases of self-harm purely to obtain medication. Most patients know exactly the medication they want in this context and it’s never paracetamol. Pregabalin, benzodiazepines, gabapentin and opioids are in high demand.
This means that clinicians need to be clinically experienced. Examination is everything as prescribing a medication can have severe repercussions. Each patient undergoes a drug test to ensure that prescribing an opioid will not fuel particular behaviours. As each prescription is highly scrutinised, Alice mentioned that documentation needs to be airtight and one must be very confident in their decisions whilst knowing the potential repercussions,
Troubling Patient Stories
Alice mentioned some really interesting points which was difficult to capture in the moment. It’s well known that many offenders have had poor starts to their lives, history of abuse and a deeply troubled upbringing. It’s very easy for clinicians to get invested into patients but Alice mentioned that in order to survive in prisons as an ACP, one has to really listen to their patients.
Listening without judgement is truly actualised in this environment and advocating for good health in an environment that doesn’t prioritise it is very hard. Ultimately, whilst they are responsible for their actions - one cannot separate their actions from the wider context of poverty, poor living standards and a system that didn’t care for them. Tackling their problem issue by issue is the key as ultimately, one hopes that once the patient is released, at least they will be healthy enough to live a fulfilling life.
Life After Prison
The short answer? It’s tough. The longer you’ve been in prison, the harder it becomes. I work in an area which has a significantly high crime rate and I often see patients who have been released from prison. Stay tuned as next weeks newsletter will be on this theme.
Until next time..
CPD Dermatology Masterclass
Rashes, itchiness, pustules, papules. These are all terms that are employed in the world of dermatology and I’m sure everyone can agree, nailing the diagnosis in dermatological terms is incredibly tough!
This is made even tougher by the fact that we live in a multicultural world and different skin disease appear differently on skin types. The stakes are high as unlike hypertension and diabetes which are “silent” diseases, dermatological illness’ have a huge impact on appearance and mental health.
We are incredibly excited to be bringing back our popular CPD Dermatology Masterclass which includes cases and presentations from various, ethnically diverse patient groups. As part of this presentation we will be covering:
Atopic, fungal and inflammatory skin disorders
Difficult to treat disorders: Acne, psoriasis, rosacea & more
Steroid, Emollients and specialist treatments
Cancers and pre-cancerous lesions: BCC, SCC, melanoma and more!
Website: www.paretoeducation.co.uk
Instagram: www.instagram.com/pareto_ed
Twitter: www.twitter.com/pareto_ed
Youtube: https://bit.ly/3DPm23c
Email: info@paretoeducation.co.uk