Acute red eye. I used to shudder at the thought of assessing eyes, not only because of the difficulty but also because of my own knowledge gaps. The reality is that such presentations are incredibly common in both primary and secondary care.
Today I want to discuss a specific cause of acute red eye.. corneal abrasions. These are often preceded by trauma to the eye, either direct or indirect but can cause severe pain in the eye.
What is a corneal abrasion?
The cornea is the most anterior portion of the eye. When injury occurs, it is often the epithelial surface of the cornea that gets “shaved off”. As it is epithelial tissue, the cornea is very good at healing any abrasions. However, secondary bacterial infections is where the problem lies…
How do they present?
Simple history includes a history of direct or indirect trauma followed by:
Red eye
Foreign body sensation within the eye
Excess watering of the eye
Photophobia
Examination is incredibly important. Despite our own personal feelings concerning eyes (ewwww!), we should be systematic in our approach to assessing the eye. Be sure to assess visual acuity, visual fields and pupillary response to light.
A useful thing to do is to flip the eye lid. This can be done with the help of a cotton bud. Here’s a useful video on this.
Tools of the trade
Examining a painful eye can be quite difficult. The eye is a tricky organ and patients can be in a lot of discomfort. There are some useful tools we can use hidden in the cupboard that will help us with examination:
Tetracaine 0.5%: This is a local anaesthetic that can be used for the eye. A drop or two will give the patient a lot of relief!
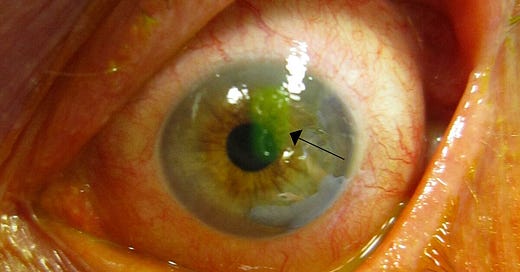
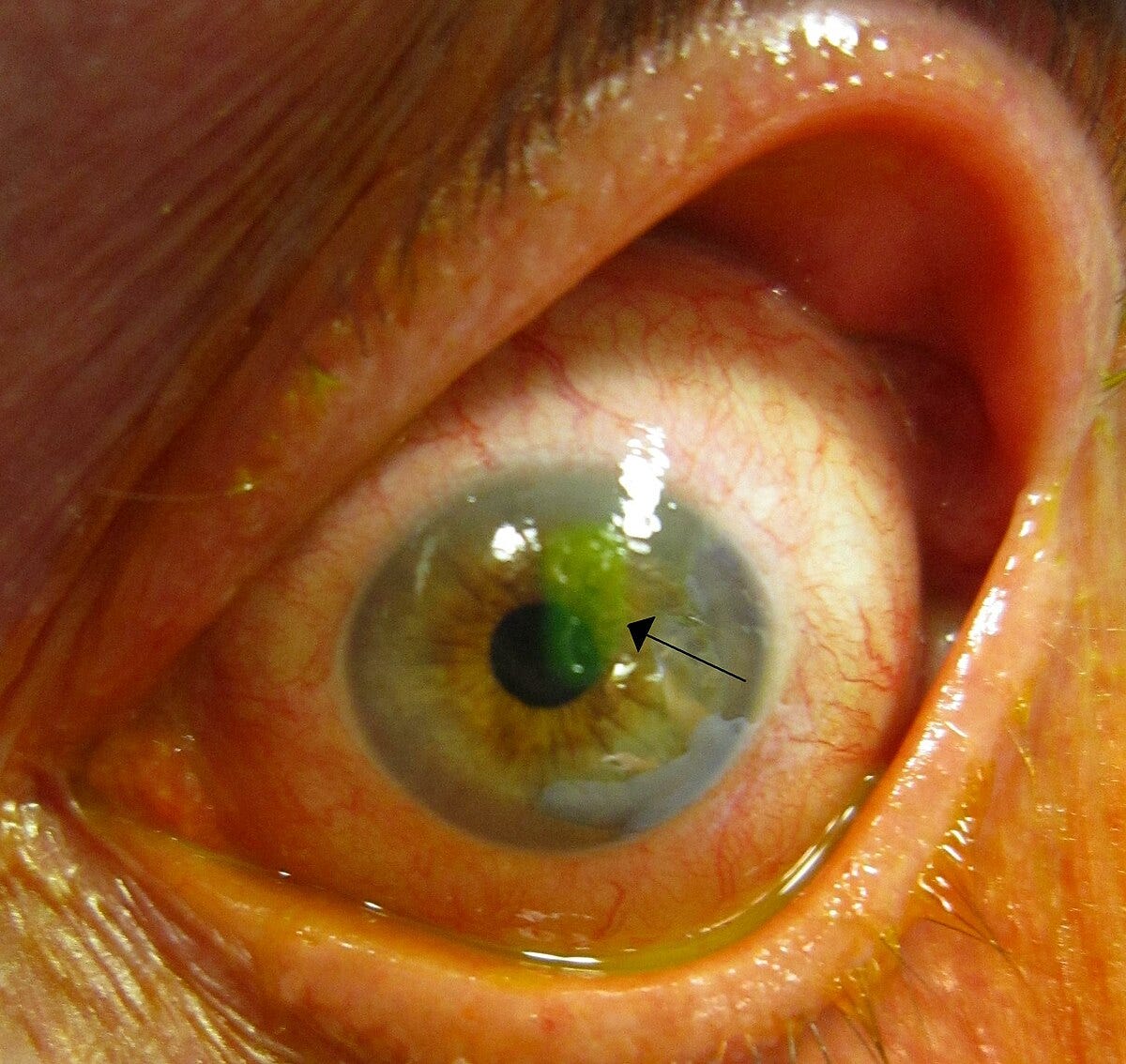
Fluorescin: This is a dye that is safe to use for the eye. It dyes the eye and elucidates any corneal abrasions that might be present.
Treatment
Once you’ve diagnosed the patient with a corneal abrasions, you must provide the treatment. Remember, the goal here is to prevent secondary bacterial infection.
Remove the foreign body if one is present
Prescribe topical antibiotics such as chloramphenicol 1% ointment or 0.5% drops (four times daily for 5 to 7 days).
Some “old-school” practitioners like to prescribe a topical steroid. However, studies show little evidence for the use of steroid eye drops.
When should I consider referral?
The vast majority of corneal abrasions are treated without any complications. However, ophthalmologists have recommended referral in certain scenarios:
Contact lense wearers: This is not an absolute referral criteria but should certainly be considered. Contact lenses by definition shave off some epithelial tissue when they are removed so it’s assumed that the depth of damage in a contact lens wearer is much more than what is seen by the naked eye. If patients have an abrasion and they have removed their contact lenses, there is also a chance that bacterial organisms could have contaminated the eye which puts patients at risk of having a secondary infection.
Foreign body visualised that you are unable or lack the confidence to remove.
Abrasion located in the centre of the eye
Reduced visual acuity
If the Abrasion is in reality an ulcer! This is important. It may be that the secondary infection has already happened and therefore, what you’re actually dealing with is a secondary keratitis (not always the case). If it looks “dendritic” then it certainly has, and will need urgent referral.
If the foreign body is a seed/grass/wood. These patients require discussion with ophthalmology as such substances carry a number of organisms making the antibiotic regimen more complicated.
So that’s a quick summary on managing corneal abrasions. We hope it’s been a good refresher for you and please do share our newsletter with others.
Are You Confident with End of Life Care?
The four largest cause of mortality are cancer, cardiovascular conditions, dementia and respiratory problems. The incidence of each of these conditions is increasingly and with that, there are more patients on the palliative care register year on year.
Palliative care services are increasingly working with primary and secondary providers to provide “collaborative care” for such patients. This means that as clinicians, our knowledge of identifying the dying patient, management and legal issues in palliative care needs to be up to date.
Join us on this CPD webinar on Sunday 4th August between 10am - 13:00. You can book here.
Check us out on our various pages
Website: www.paretoeducation.co.uk
Instagram: www.instagram.com/pareto_ed
Twitter: www.twitter.com/pareto_ed
Youtube: https://bit.ly/3DPm23c
Email: paretopaeducation@gmail.com