The title. I know. You’re thinking emboli right? Not a bad guess.
Don’t worry if you weren’t by the way as I certainly wasn’t…
There are some odd cases when severe sepsis results in the formation bacterial emboli which fire off into the peripheral circulation causing all sorts of madness. However, I want to share a case which is actually simpler..
Sepsis is pretty common. I think we perhaps overuse the term but certainly patients with infections come in their droves this time of the year. I recently saw a 84-year-old gentleman who normally lives with his wife.
He woke up in the morning and got up to use the toilet but simply fell to the ground. He was blue like a smurf and his wife immediately called 999.
The paramedics found his oxygen levels to be 71% on air. Using the classic ABCDE assessment framework they whacked him on 15L oxygen via a non-rebreathe mask. His blood pressure was low and his HR was through the roof – in fast atrial fibrillation (AF) actually. They pre-alerted the local A&E department where little ol’ me was the senior doctor in the high dependency unit.
It was a busy day and “here we go again…” is what I thought.
The patient was brought in – he didn’t look well. His GCS was probably 9 but he was maintaining his own airway. I tried to talk to him but there was no response. We proceeded to do some blood tests and I did an ABG.
Here are the results on 15L oxygen
pH - 7.48 (7.35-7.45)
PO2 10.1 mmHg (7-10 mmHg)
PCO2 2.3 mmHg (3.5-4.5 mmHg)
HCO3 27 mEq/L (22-26 mEqL)
Now this looks like a severe type 1 respiratory failure. I spoke to the patients wife who said that he had been coughing a few days prior so perhaps this is all a really bad chest infection? I prescribed some antibiotics and some fluids after taking blood cultures and I then went onto see the next patient.
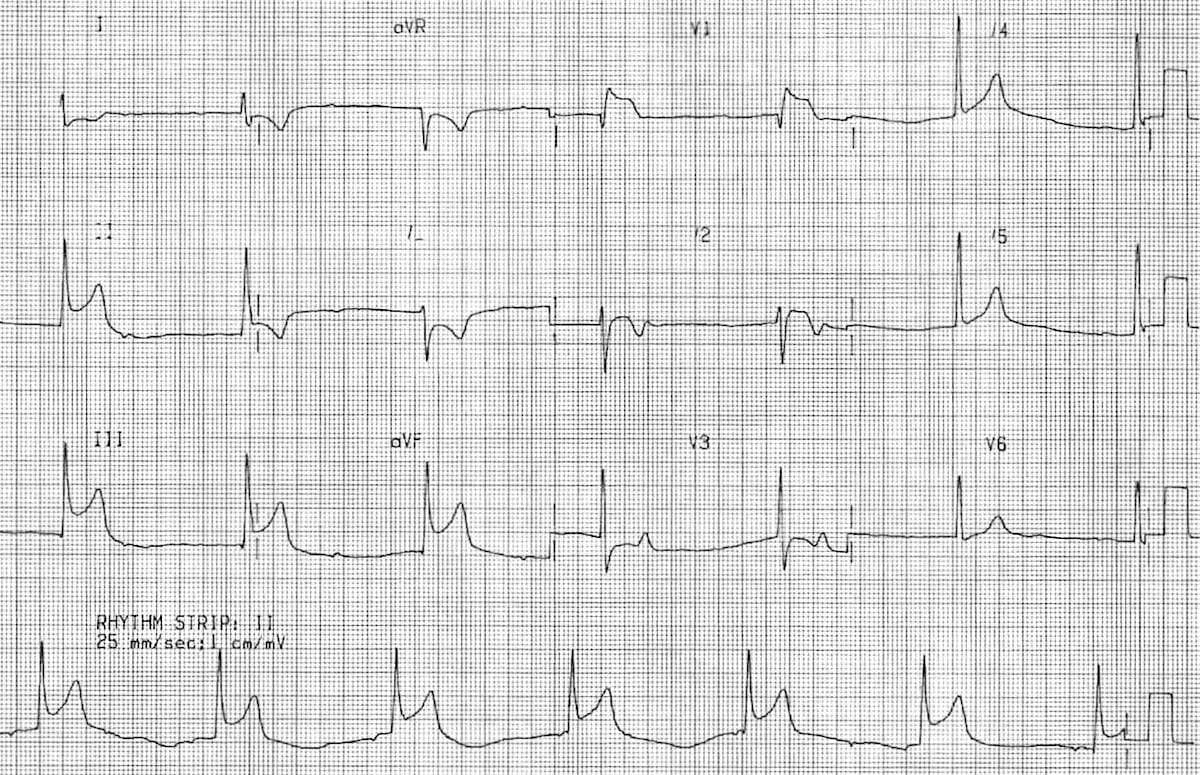
After a few minutes the nurse looking after the patient approached me with an ECG to sign. Quite a routine thing in A&E especially because his heart rate was 151! I looked at the ECG and thought “Oh S***”.
He had ST elevation on his inferior leads.
His GCS was still quite low. I added on a troponin to his blood tests and called the elderly care registrar to see if we could anything else.
This patient was likely to have had a type II MI which is an MI secondary to ischaemia as a result of increased oxygen demand. We decided to give him some aspirin (just incase there was a clot) and treat his sepsis. After a bit of panic I composed myself and ofcourse in the meantime, there were two new patients who had arrived!
Things were fine for a few hours until something else happened. His GCS dropped to 5 and he had no muscle tone on his right arm and leg. We weren’t not quite sure when this started as on my initial examination he was certainly moving his limbs. It was clear that he had a stroke and this mans prognosis was getting worse and worse.
There was no DNACPR on him at the time. I mean.. he was an independent, fit and well gentleman with very few co-morbidities. I placed a nasopharyngeal airway in his nose and called anaesthetics. He was too unstable for a CT scan without airway support and anaesthetics kindly came and dealt with him.
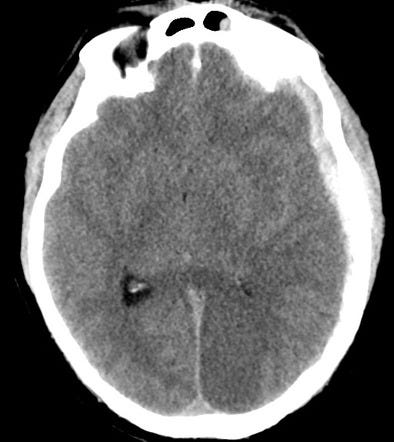
The CT showed some changes in the posterior lobe bilaterally.
I called the stroke consultant to get his thoughts and the stroke team came and saw him. There was somewhat of an onset time so he could be considered for thrombolysis but ofcourse with everything else going on – it would be risky.
We decided to hold fire. I was tired and my head was hurting because of all the thinking and running around. But what actually did happen?
It’s quite exciting for us to think about cool cases such as septic emboli but such instances are rare. This cascade of pneumonia —> inferior MI —> stroke occurred purely as a result of hypoxia. Hypoxia really does kill and in just 6 hours, this patient has gone from being completely independent to a GCS 5.
The ensuing discussion with the family was tough. "Where do I even start?” I thought. How would I explain that their relative who was having dinner with them yesterday now can’t speak to them? It was one of the hardest DNACPR discussions ever.
It was tough. It was emotional, but the family understood the situation. They were in shock but felt that the sudden nature of the patients deterioration was probably how he would have wanted to go in the first instance. We decided to make comfort the priority and withdrew oxygen and the patient shortly passed away.
Never will I overlook sepsis again…
A pneumonia is never just a pneumonia as the associated hypoxia can cascade into a wide array of medical problems. There’s a reason why we always emphasise the sepsis six. Whilst it is difficult to initiate it in a time sensitive way it is the most effective tool we have to when battling severe sepsis. In this case the oxygen would only delay the inevitable but in the case of thousands of others it potentially saves them from severe morbidity or mortality.
Pareto Pixel
Check out our Pareto Pixels with our latest video covering TB pathophysiology and investigations in less than 3 minutes!