I recently spoke with a consultant in metabolic medicine who shared his insights on running Tier 3 obesity clinics. Obesity is a major issue in the UK, with 28% of the population classified as obese. It is closely linked to social deprivation, with the highest rates found in some of the most disadvantaged areas. Beyond its well-documented impact on physical health, obesity also carries significant psychological consequences, contributing to economic inactivity among affected individuals. Conditions such as depression, diabetes, and osteoarthritis are just a few of the many health issues that arise as a result.
As a consequence, the NHS spends £11.4 billion annually on obesity-related illnesses. While efforts have long focused on lifestyle interventions, including behavioral changes and dietary adjustments, progress in effectively treating obesity has been slow.
That is, until recently. The introduction of Mounjaro (Tirzepatide) has been a game changer. Every day, we receive at least two to three letters from private providers informing us that patients have started on Mounjaro. The treatment costs approximately £200 per month, with a minimum recommended duration of two years—amounting to nearly £5,000over that period.
So, what makes Mounjaro so significant? Does it actually work? These are some of the key questions we’ll explore in this week’s newsletter.
What is Mounjaro?
Tirzepatide (sold under the brand name Mounjaro) is a medication that helps with weight loss by mimicking two key hormones involved in appetite regulation and blood sugar control:
GLP-1 (Glucagon-Like Peptide-1) receptor agonist – This hormone slows down stomach emptying, reduces appetite, and increases the feeling of fullness after eating. It also enhances insulin secretion, lowering blood sugar levels.
GIP (Glucose-Dependent Insulinotropic Polypeptide) receptor agonist – This hormone improves how the body processes fat and enhances the effects of GLP-1, further suppressing appetite and promoting fat loss.
How It Works for Weight Loss:
Reduces hunger – It decreases cravings and helps people eat smaller portions.
Increases fullness – Slows digestion, keeping food in the stomach longer, leading to prolonged satiety.
Improves fat metabolism – Enhances how the body processes and burns fat.
Lowers blood sugar levels – Helps regulate insulin and glucose, which can contribute to weight management.
Its actions on GIP receptors is what gives it an edge over other injection therapies like semaglutide (Wegovy). This allows Mounjaro to be more effective as well as enabling longer term effects (which we will cover shortly).
How Effective is Mounjaro?
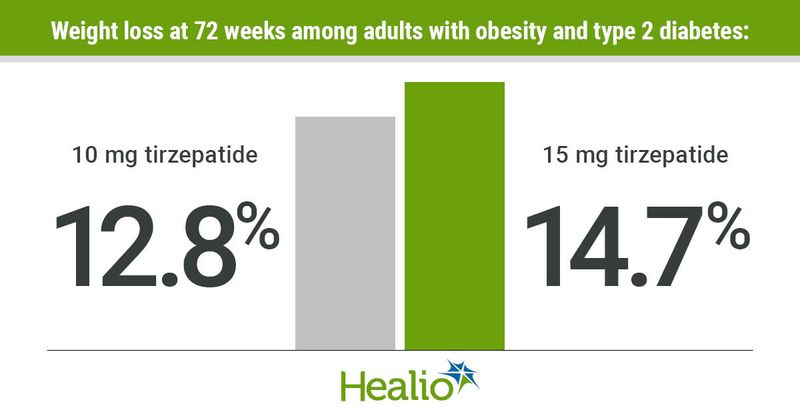
The short answer? Extremely effective. Clinical trials, including the SURMOUNT trials, have shown that tirzepatide can lead to substantial weight loss, with participants losing 15-22% of their body weight over 72 weeks. This makes it one of the most effective weight-loss medications currently available.
Mounjaro (tirzepatide) is generally well tolerated but can cause nausea, vomiting, diarrhea, constipation, and reduced appetite, especially early on. Less common side effects include reflux, dizziness, and injection site reactions, while serious risks (though rare) include pancreatitis, gallbladder issues, and severe allergic reactions.
However, concerns remain about its long-term effects. A five-year clinical trial is in the works to assess potential risks, but for now, there is no restriction on how long Mounjaro can be prescribed. This is largely because, once patients stop taking Mounjaro or Wegovy, they tend to rapidly regain the weight they previously lost.
Which brings me to the next topic… the fine print.
The Fine Print
The consultant I spoke with works in both the private and public sectors. Unfortunately, the NHS lacks the resources to roll out Mounjaro on a large scale—primarily due to the fine print involved. Most patients with obesity have health behaviors that reduce the likelihood of Mounjaro being effective.
Take the SURMOUNT trial, for example. While it demonstrated remarkable weight loss, participants weren’t just taking Mounjaro—they were also following a 500-calorie daily deficit and engaging in 150 minutes of exercise per week. This is what I mean by the fine print—successful treatment requires dietitian support and regular follow-ups, something the private sector often doesn’t provide.
The second issue? Cost. As mentioned earlier, the manufacturer of Mounjaro recommends that patients remain on the treatment for at least three years. That adds up to nearly £14,000—a sum that is difficult for most people to afford. As a result, some patients choose to undergo weight-loss surgery abroad, which comes with its own risks and complications—though that’s a topic for another time and not something we’ll be covering in this week’s newsletter.
The Future of Weight Loss Treatment in the NHS
For the NHS, the real challenge lies in the fine print.
We already know that obesity rates are highest in areas of socioeconomic deprivation—precisely where people are least likely to afford private treatments. These areas also have fewer primary care clinicians, with some of the highest patient-to-clinician ratios in the country. At the same time, patients in these communities often struggle to implementthe lifestyle and dietary changes necessary for Mounjaro to be effective.
The NHS has developed a 12-year implementation plan aimed at targeting high-risk obese patients, but without the necessary resources to fully support it. There are other proven weight-loss interventions—such as high-intensity interval training, low-carbohydrate diets, and pharmacological options like Wegovy. Yet, despite these alternatives, the focus continues to shift toward Mounjaro, even though the support systems required for its success remain inadequate.
With Mounjaro becoming more widely available, access to Tier 3 weight management services may improve. It’s even possible that Mounjaro will eventually be offered in primary care settings. But for those who start treatment privately, it will likely be primary care clinicians who are left to pick up the pieces—yet again.
For a deeper read on some of the above, we’d recommend referring to this recent BMJ article on the topic.
CPD Point of Care Masterclass
Point of care testing is the future. From nasal swabs for flu to urine dips for UTI, we’ve been using frontline testing for a long time. However, this has now extended further to more complicated investigations such as ABG, VBG, CXR/AXR, ECGs and more!
This CPD accredited masterclass is perfect for front line clinicians that use investigations to make critical decisions such as admission, onward referral or discharge. On this course we will cover:
- Understanding the role and use of POCT in urgent and acute care
- Key ECG Interpretation
- Interpreting blood gases (ABG AND VBG), urinalysis and key blood tests
- POCT scoring criteria for minor illness'
- Imaging including CXR, Abdominal XR, CT head & more
As part of this you will receive
LIVE and RECORDED ACCESS for 60 days incase you can’t make the live event/want to watch again
CPD accredited certificate
This course will be held on Sunday 9th March 2025. If you can’t make the live course, you will also receive RECORDED access :). You can book here.
Website: www.paretoeducation.co.uk
Instagram: www.instagram.com/pareto_ed
Twitter: www.twitter.com/pareto_ed
Youtube: https://bit.ly/3DPm23c
Email: info@paretoeducation.co.uk