As clinicians, empathy is the bedrock of our practice. However, there are situations where it can be quite hard to empathise, particularly when you don’t share in the persons suffering or are unable to understand why they feel the way they do.
For a long time, chronic pain was one of those things.
I have been in pain before and have certainly been through some experiences where my emotions have been tested but such experiences have been short lived. Chronic pain affects between a third and half of the population globally. It is defined as pain that is experienced on most days for more than three months causing restriction in at least one activity. It is estimated that 22-50% of GP consultations are related to pain.
These are quite startling stats and it can certainly be frustrating dealing with chronic pain precisely because we might not understand it. In this issue, I wanted to shed some light on chronic pain and how we can better manage patients affected by it.
What is our current practice?
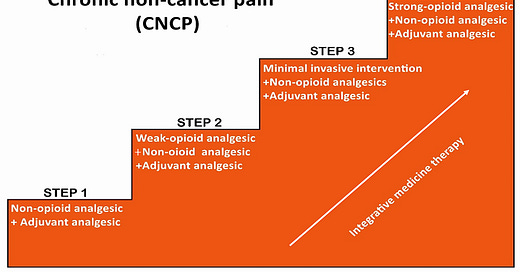
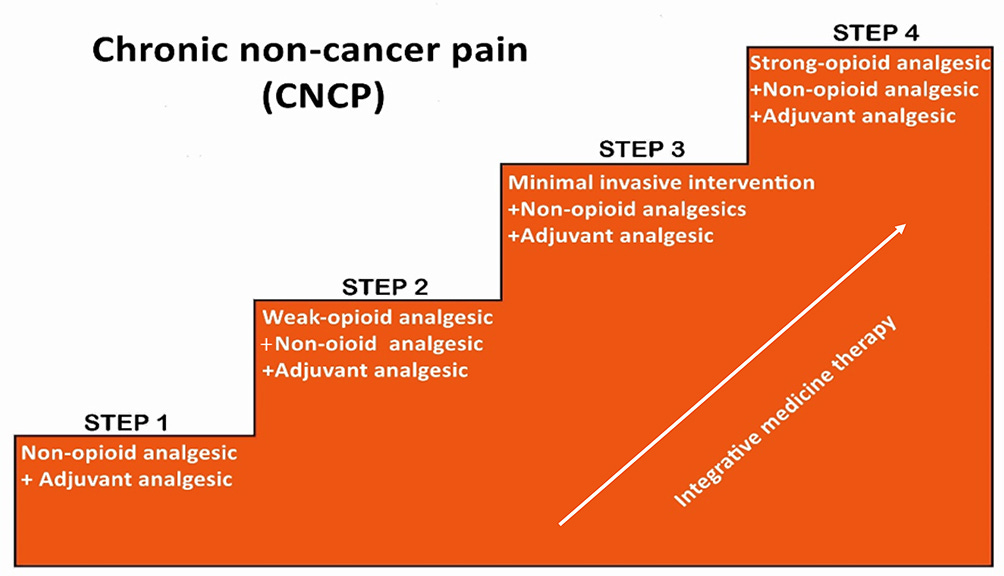
Before I started to look into this, my strategy was to simply cycle through analgesia. I would move from class to class and found that medication, including drugs such as amitryptiline did very little to heal the patients pain. I’d also find myself cycling through lots of blood tests, sometimes repeating tests that have been done a few weeks ago only to find myself hitting a brick wall. This is where we start to disassociate with our patients struggles as an abyss of misunderstanding develops. All of this simply results in:
- Clinician frustration
- Patient frustration
Why does chronic pain occur?
Studies have found that chronic pain usually occurs after some sort of acute pain or disturbance. Suppose a patient has a wrist sprain. We would typically assess and advise a rest, ice, compression and elevation approach. However, somewhere along the line the following changes occur that results in a simple muscle sprain not being so simple:
- The patients nerves re-wire incorrectly,
- The nerves start to misfire
- The brain perceives simple sensations such as touch incorrectly.
For more information, this is a good video on understanding chronic pain from an anaesthetist.
How does this change our practice?
Well.. Now that we understand that chronic pain is a result of the above, we can start to think about how we can change our approach. A good start would be to think about broader factors affecting the health of our nerves. For example:
Strengthening nerves with nutrition
Providing them with sufficient rest through good sleep
Encouraging neuroplasticity (re-wiring) using exercise
And helping them to appropriate stimuli properly through psychological therapies and counselling.
How do we achieve the above in a 10-20 minute consultation?
I get it. It’s hard to do all the above in a GP/secondary care setting. However, we can certainly start the process by exploring something powerful called “patient role.”
Patient role refers to the primary role a patient sees themselves playing which then allows us to explore how their illness has impacted them in fulfilling this role.
For example, I’m a father and I know that if my health was impacted and I could not work, it would really put a downer on me. Everyone’s different but this is important to me. The thing is, you might not be able to get on top of the pain but trying to understand the patients role and the impact of their pain can start the process of helping to treat the patients chronic pain. If a patients’ back pain has impacted the their role as a mother, connecting with this is vital as you help to validate their concerns which can really enhance the chances of your patient engaging with self-management strategies.
Practically speaking, asking simple questions as “what’s important to you?” and “how has your pain impacted your ___” has done my relationship with patients wonders. It is precisely these questions that enabled me to then explain some management strategies.
I’d really recommend reading this article titled Chronic pain: definitions and diagnosis | The BMJ It expands a great deal on what I’ve written above.
Check out our CPD Calendar
Our next event is TONIGHT covering Angina, ACS and its complications. However, don’t miss this months special event where we deliver a 3 hour webinar on ECG interpretation. We have packed it with theory, case studies and worked examples to help solidify your understanding of ECGs.
On top of this, we also give you a FREE E book as further reference material. All this for just £9.99! Visit www.paretoeducation.co.uk/courses for more information
Check us out on our various pages:
Website: www.paretoeducation.co.uk
Instagram: https://tdy.lol/lQSxv
TikTok: https://tdy.lol/AJdzQ
YouTube: https://tdy.lol/ZEoOt
Newsletter: https://tdy.lol/WnTBR
LinkedIn: https://tdy.lol/efLOB