Here’s a case I recently encountered. It stumbled me and I’m sure you’ll see why…
I recently assessed an 8 year old girl who presented with urinary trouble. Her mother explained that the patient was having urinary dribbling throughout the day.
I enquired as to whether that was just during the day and she affirmed this. There was no history of any accidents either during the day or night and no signs and symptoms of a urinary tract infection. When asked to quantify how much urine was leaking, the patient said a few drops but sometimes more which prompts her to get changed.
Mum was worried as she was worried that this may get worse and subsequently affected her daughters performance at school as the holidays were almost over. “Do you have any specific concerns?” I asked. Mum mentioned that they had seen a doctor abroad who suggested a vesicoureteral reflux. “Oh dear..” I thought to myself.
What is a VUR?
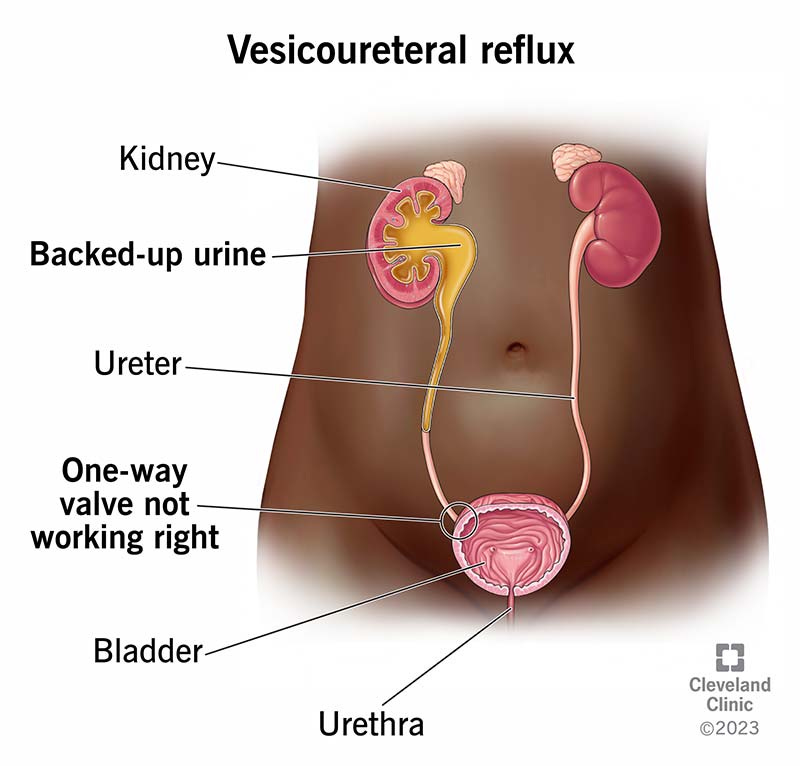
Vesicoureteral reflux (VUR) is a medical condition where urine flows backward from the bladder into the ureters and sometimes into the kidneys. Normally, urine flows in one direction: from the kidneys, through the ureters, to the bladder, and out of the body. However, in VUR, this one-way valve between the bladder and the ureters is defective or weakened, allowing urine to move back up.
There are two types of VUR. Primary VUR normally starts very early on in life and is due to a developmental abnormality in the valves and ureters, leading to the back flow of urine. So when children are being toilet trained, parents may realise that they’re having no luck and despite being toilet trained, children may be having significant accidents and trouble getting to the toilet in time.
Secondary VUR is due to a structural abnormality. This means that treatment of this requires identification and either medical or surgical management. Some common causes include:
- Repeated urinary tract infections (UTIs) causing damage to the valves and urethra
- Neurogenic bladder
- Bladder outlet obstruction
- Posterior urethral valves
- Increased bladder pressure
How do we investigate patients with suspected VUR?
The first step is to perform an ultrasound scan of the urinary tract. Whilst it may now demonstrate the exact cause of the back flow, it provides “secondary signs” to suggest that a VUR is present. This includes dilated ureters, bladder thickness and even hydronephrosis. In any case, patients with a strong suspicion of a VUR are referred for a more definitive investigation such as voiding cystourethrogram (VCUG).
What happened to this patient?
My index of suspicion was quite low for this patient. I did order an ultrasound scan which turned out to be completely normal. As there was no history of significant accidents or bedwetting it was always unlikely to be a VUR. I sought to get some A&G from paediatric urology who helpfully suggested a diagnosis of “overactive bladder.” So this is where my focus was directed to.
We tend to think about overactive bladder in elderly patients but it can certainly occur in children too! It’s when the bladder muscles contract before they are ready to empty.
So how do we treat a child’s overactive bladder? Think of the causes
Is the patient constipated?
Is the patient not drinking enough? Concentrated urine can irritate the bladder lining.
What are they drinking? Fizzy drinks, caffeine or chocolate drinks can irritate the bladder
Are they holding on for too long instead of going to the toilet?
Is there a UTI? Don’t forget your basics of doing a urine dip!
So most issues with urine in young children is normally down to lifestyle and behavioural factors. It’s important to not be dismissive and take a patients concerns seriously. An USS is a good introductory investigation that can provide reassurance if normal, especially If your impression is overactive bladder. Reassure patients that overactive bladder can be treated. The trick here is to be comprehensive and not miss out the simpler, lifestyle causes of bladder irritation.
Until next time…
Announcing the launch of our CPD calendar
After the success of our CPD courses throughout the year, we have taken your feedback onboard and re-vamped our upcoming calendar. Here is what we’ve done:
We have organised CPD courses on the topics that you requested to help address weaker areas in order to help you upskill.
We have invited specialists in each field to deliver their topics. We have a line up of gynaecologists, gastroenterologists, physiotherapists (ACP) and others.
You can now watch each CPD course live AND on-demand. You will have EXCLUSIVE access to each event for 60 days so you can watch it in your own time.
All our courses are externally accredited by the CPD company so you can complete your curriculum requirements.
Join us for our first event on Sunday 22nd September where we cover CPD Women’s Health. Our guest lecturer, Dr Farhat Bibi a specialist registrar in obstetrics and gynaecology will provide teaching on tricky practice areas such as:
Managing PV bleeding in the acute setting
HRT counselling, prescription and follow up,
Endometriosis & uterine fibroids: updates in management
Gynaecological malignancies
You can book here: https://www.paretoeducation.co.uk/service-page/cpd-women-s-health-masterclass
See you there :)
Check us out on our various pages
Website: www.paretoeducation.co.uk
Instagram: www.instagram.com/pareto_ed
Twitter: www.twitter.com/pareto_ed
Youtube: https://bit.ly/3DPm23c
Email: paretopaeducation@gmail.com