Why Quality Improvement Projects (QIP) Are Worth Your Time
Why QIPs make you stand out as a clinician
When I was training as a medical student, the focus was always on doing audits.
I remember being that keen student who would ask placement supervisors if there were “any audits going around.” Medicine is a highly competitive space, and audits were a way by which we could stand out when applying to specialties.
Things changed around 2016 when the NHS moved away from audits and turned towards quality improvement projects(QIP). These also became infused into masters’ degree programmes such as an MSc in Advanced Clinical Practitioner and Physician Associate studies, making QIPs the industry standard for improvement.
The move from audits to QIPs made a lot of sense and I want to explain why this change occurred. This issue will cover:
Why you should involve yourself in QIPs
How you can effectively involve yourself in QIPs.
So brace yourselves!
Why QIP?
Audits have always served an important purpose. They are carried out to assess where a service is at, define an intervention to better that service and subsequently review the result to show how the intervention helped. The problem with this is:
After the initial success of the intervention the next point of re-evaluation would be a year later where it would be found that the initial improvement had vanished...
The interventions would often be limited to posters, IT prompts and emails which eventually became background “noise".
Audits produced no long-term culture change.
Overtime, carrying out audits became less about patient safety and improvement and more as a “tick-box” exercise.
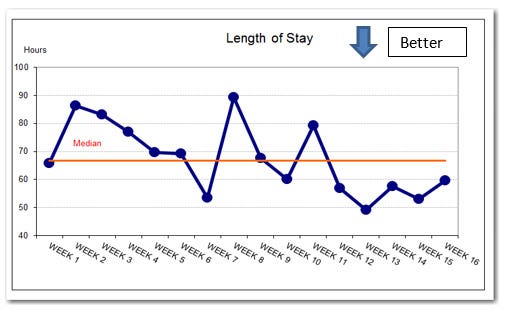
QIPs were introduced to correct this. It focussed on evaluating an intervention over time using “run charts” and instituting phases of intervention as opposed to relying on only a single intervention. The goal of this is to ensure that an intervention is run over a substantial period of time to institute a lasting, culture change in an organisation or department.
Why You Should Involve Yourself in Quality Improvement
As a clinician, we are all expected to make an improvement either in the field of research or clinical practice. We are practical people, so instituting change and improvement comes quite natural to us.
With patient safety in mind, we want to improve practice so that we can serve our patients more effectively. In addition to this, most appraisals nowadays mandate a “quality improvement” project or activity. Organisations such as practices and NHS Trusts like to hire people who are practical, problem solvers.
I’ve completed a total of NINE quality improvement projects in my clinical career so far and each has brought something different to the respective departments. Here are some of the QIPs I’ve completed:
Encouraging clinicians in a general surgical unit to consistently use the GLASGOW score for patients with acute pancreatitis. This is to better anticipate ICU admissions.
Teaching nurses on a breast surgery unit on how to better assess post surgical wounds. This has led to “criteria-led discharges”, reducing workload from doctors.
Designing a service user questionnaire for blind patients in an ophthalmic unit to allow the department to better evaluate its service.
Cleaning the registrars clinic room in a GP surgery to create a happier working environment.
Now no-one is asking you to do nine but just doing one of the above would have been sufficient. They demonstrate initiative, care, ambition and leadership. These are qualities that are necessary to be an effective clinician as well as a valuable employee in any organisation.
How Do I Get Involved in a QIP?
This can be thought about in the following way.
“What troubles me in my day-to-day practice and how can I change this in the long term?”
The last example in the list above was down to my frustration of working in a messy room. The room was full of old textbooks, posters and other sheets of information that no-one cared for. I approached my line manager and informed him of my intention and that was all that was needed.
I wore some gloves and cleared out the workspace and created some guidance on how often charts needed to be changed on the display board. The key is to find a problem and work backwards in defining how you can solve it. There are a ton of useful resources, some of which are as follows:
This is an awesome article in the BMJ that goes into further detail on what I have explained above.
The Improvement Academy. This is a useful website created in collaboration with NIHR that explains the principles of quality improvement.
If you’re after a step-by-step guide then check out this report published by The Health Foundation. It is an easy but detailed read.
It would be great to know about your QIP journey so far. I intend to go into some of the core principles of QIP in future newsletters.
Until next time!
What’s On?
Our ECG Masterclass is BACK and this time we’ve made it even better. We will cover the basics of ECGs, lay out our FULL PROOF method of interpretation and explore multiple examples. We also have a special section on 24-hour tape results and interpretation.
This masterclass will be perfect for students and qualified professionals and there will be lots included for both beginners and experts. Oh.. and to top it off, you will also get an ECG e-book written by us :)
Check us out on our various pages
Website: www.paretoeducation.co.uk
Instagram: www.instagram.com/pareto_ed
Twitter: www.twitter.com/pareto_ed
Youtube: https://bit.ly/3DPm23c
Email: paretopaeducation@gmail.com